Why Has Covid-19 Caused So Many Deaths?

The COVID-19 pandemic has left an indelible mark on our world, challenging nations, communities, and individuals’ resilience. With its relentless global spread, the SARS-CoV-2 virus,…

The COVID-19 pandemic has left an indelible mark on our world, challenging nations, communities, and individuals’ resilience. With its relentless global spread, the SARS-CoV-2 virus,…

The COVID-19 pandemic has swept across the globe, leaving no corner of the world untouched by its profound impact. It has forced humanity into an…

The COVID-19 pandemic, a global crisis of unparalleled proportions, has not only reshaped our lives but also sent shockwaves through the world’s economies. As nations…

The COVID-19 pandemic has left an indelible mark on the global landscape, reshaping every facet of our lives, including the way we earn, spend, and…

In the face of a global pandemic that has reshaped the very fabric of our lives, it’s become abundantly clear that the battle against COVID-19…

The COVID-19 pandemic has indelibly changed our collective history, leaving an indelible imprint on how we live, work, and connect. So, how did the pandemic…

The COVID-19 pandemic was a tough time for everyone. It didn’t just affect our bodies. It also made us feel very stressed, lonely, and worried.…
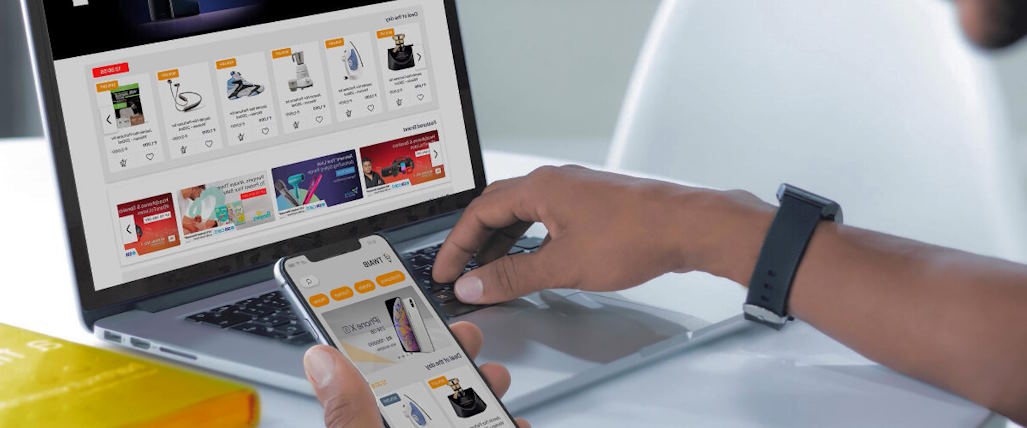
The COVID-19 pandemic posed unprecedented challenges to businesses across the globe, reshaping the landscape of commerce in ways unforeseen and unparalleled. As the world grappled…

The COVID-19 pandemic triggered an unprecedented transformation in the world of work. Almost overnight, businesses tried to provide remote work to respond to the urgent…

It’s not a secret that the pandemic brought significant disruptions to various aspects of our daily lives, but perhaps none more profoundly affected than education.…